Summer sports games and practices are well underway. With the excitement of another season comes the dangers of playing in hot and humid conditions. There are 3 forms of exertional heat illness that players, parents, and coaches should be familiar with. These are heat cramps, heat exhaustion, and heatstroke.
3 Forms of Exertional Heat Illness
1. Heat Cramps
Heat cramps are the least serious. They involve painful cramping of large muscles. They usually affect your calf muscles. Sodium loss and dehydration from high rates of sweating lead to heat cramps.
Treatment of heat cramps involves moving the athlete to a cooler environment. It is also important to administer fluids like sodium-containing sports drinks (Gatorade). The best prevention is remaining hydrated before and during practices. Liberal use of sodium-containing foods or beverages can also help.
2. Heat Exhaustion
Heat exhaustion is a more serious disorder. Signs of heat exhaustion are fatigue, dizziness, nausea, vomiting, fainting, and a weak rapid pulse. In these cases, the athlete’s cardiovascular system is unable to meet the needs of the body as it becomes dehydrated.
Dehydration caused by fluid loss from sweating leads to heat exhaustion. Athletes who are unfit or not acclimated to the heat are more susceptible. Treatment involves resting in a cool environment with the feet elevated to facilitate blood return to the heart. It is also important for the athlete to drink fluids. Cold water or a sodium-containing sports drink is best.
3. Heat Stroke
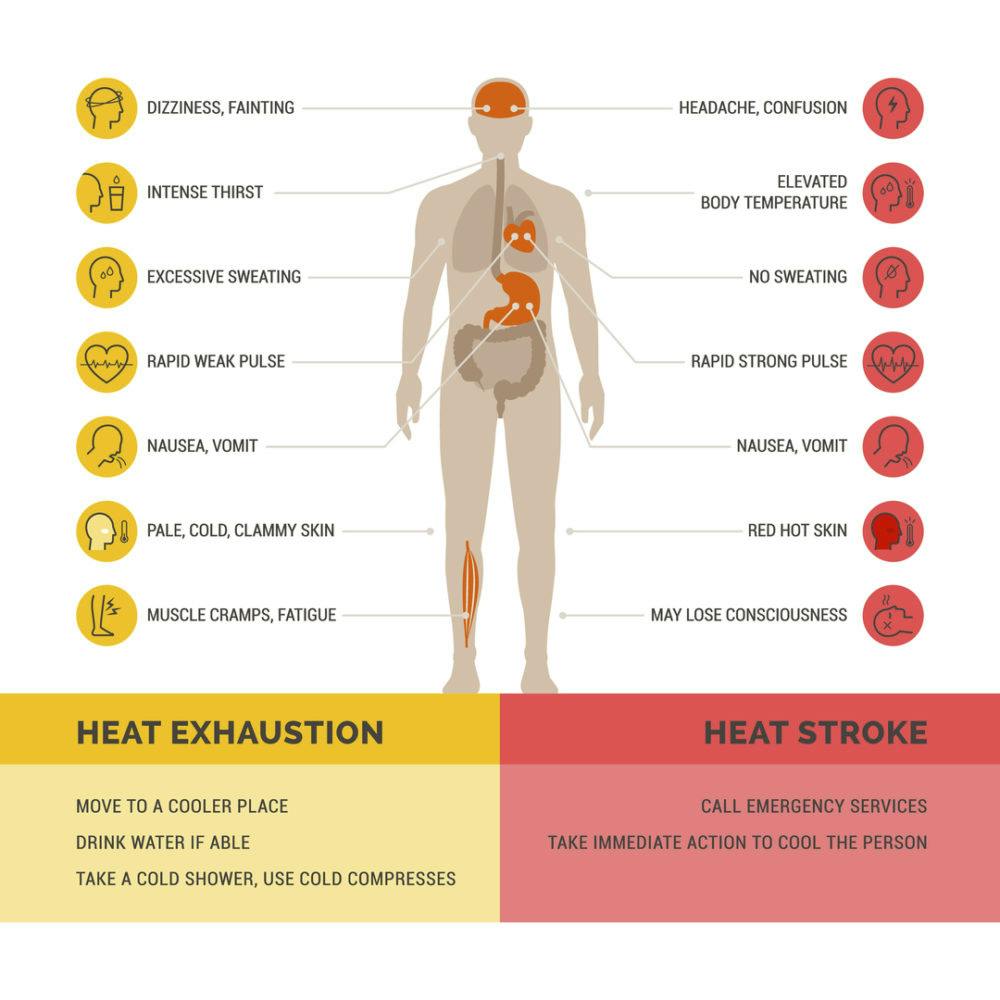
Heatstroke is a life-threatening disorder requiring immediate medical attention. An inability to control core body temperature becomes a medical emergency. A core body temperature exceeding 104 degrees, confusion, disorientation, and unconsciousness are hallmark signs.
If left untreated, body temperature will continue to rise progressing to coma and even death. Call 9-1-1 when heat stroke is suspected. Rapid cooling of the body in an ice bath is the best form of treatment. If cold-water immersion is unavailable the athlete should be wrapped in cold wet sheets while others fan the body.
The Impact of Humidity

High humidity means the air contains many water molecules. In these instances, the air cannot accept much more water. During exercise in the heat, excessive body heat is lost through the evaporation of sweat at the surface of the skin. If humidity is high, sweating will be much less effective in releasing body heat because evaporation is inhibited.
Even though sweat secretion will continue during the activity, without evaporation the rate of core body temperature will continue to rise. Therefore, high humidity increases the likelihood of experiencing any of the 3 forms of exertional heat illness.
Common Sense Steps to Prevent Heat Illness
Athletes can take preventative steps to minimize the effects of playing in hot environments. Strategies that promote heat adaptation assist with an athlete’s ability to tolerate and perform in hot and humid environments.
Adaptation requires a series of gradual progressively increasing temperatures in order to produce sufficient adaptations. Longer and more frequent heat exposures produce heat adaptation benefits resulting in the greatest capacity and performance benefits. Regimens lasting more than 14 days show the greatest benefits.
Coaches and parents should take preventative steps when threatening conditions are present. Practices in the early morning or evening can avoid the severe heat stress of midday.
Fluids should be available and athletes should be given drink breaks every 15 to 30 minutes. Weighing athletes before and after exercise can help estimate individual sweat rates and fluid needs. Fluids containing electrolytes and carbohydrates can provide benefits over water alone.
Light-colored, lightweight, loose-fitting clothing should be worn whenever possible. And finally, heavy use of equipment (i.e., football pads and helmets) should be minimized or avoided early in the practice season when athletes are not yet fit or acclimated to the heat.
If you have more questions about how to exercise in the heat, contact one of our physical therapists.

