Arthritis pain affects over 50 million people in the U.S. Osteoarthritis is the most common form of chronic painful joint disease. The most frequently affected joint is the knee. Up to 1 in 8 men and women over the age of 60 have painful knee arthritis. It is also common in the hips, spine, and hands. Arthritis is a leading cause of impaired mobility and disability in older adults.
Many people believe arthritis is a natural part of aging and little can be done for it. This belief is false and unhelpful. Understanding what arthritis is and why it can be painful will provide you with a sense of control.
The purpose of this article is to teach and inspire you to take action so you can manage your arthritis without medication, injections, or surgery. We will start by explaining how the joints and nervous system change in people with arthritis. We will also briefly explain several proven approaches to help you with your arthritis pain.
Structural Changes in Joints with Arthritis
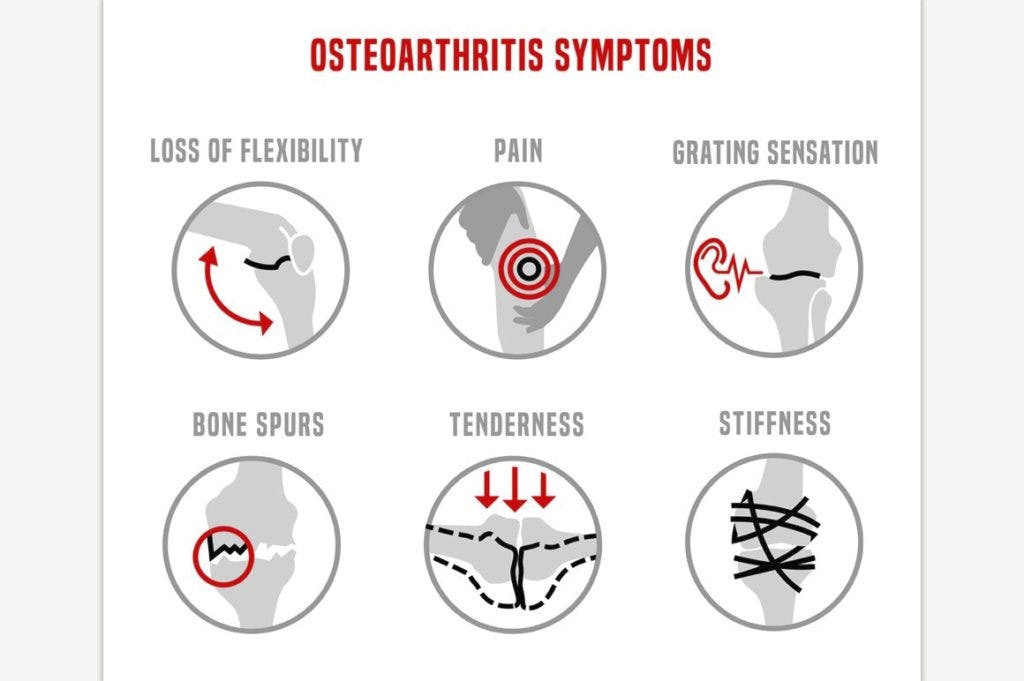
In a typical joint, a layer of cartilage protects and cushions the ends of your bones. The hallmark sign of arthritis is a loss of cartilage on the ends of each bone. Cartilage has no nerve supply so it cannot be the direct source of your pain. In severe cases, the bone underneath your cartilage can trigger pain. More often inflammation within the lining of your joints and ligaments triggers pain.
Over time, the inflamed joint lining and ligaments thicken and create stiffness. This results in a cycle of pain and stiffness which begins to limit your use of the affected joint. Reduced activity leads to weakness of the surrounding muscles. Muscle weakness contributes to increased stress through your arthritic joint. The vicious cycle of inflammation, stiffness, pain, and weakness leads to more pain and a sense of hopelessness.
Changes within the Nervous System from Arthritis
Pain is a protective mechanism inherent in all of us. It helps us escape danger. However; pain is complex and sometimes can be overly protective when no danger is present. The type, duration, and intensity of pain rarely can be explained by an x-ray or MRI.
This is because pain results from the interaction of many different factors. These factors include changes in and around the joint. However other social, cultural, and psychological factors, including underlying anxiety and depression, are always interacting to produce pain.
The term “neuromatrix” has been coined by world-renowned pain expert, Dr. Ronald Melzack. This concept explains the complex interplay between the factors which lead to pain.
As a result of an injury or inflammation, nerve endings within your joint become stimulated. Once stimulated, signals are transmitted up your spinal cord to your brain. Your brain then processes these signals along with your past and present experiences, thoughts, beliefs, cultural factors, and social or work environment.
After considering all these influences, the brain determines whether or not you are in danger and if so, how much danger. If your brain perceives a serious threat, it sends signals back down to your arthritic joint. These signals result in an unpleasant experience of pain. If no threat is determined, your brain produces no signals to create pain. Read on and we will discuss how you can reduce any perceived threat.
How to Manage Pain from Arthritis
Understanding why arthritis causes pain allows us to identify treatments that can help. During acute and painful times, treatments focus on reducing inflammation and stiffness. Then gradually exercises to improve strength and mobility are added. Finally, a holistic approach including the body and mind is needed to achieve long-lasting improvements in pain from arthritis.
Passive Treatments to Reduce Pain and Stiffness
Passive treatments provided by a healthcare professional or applied to a painful area can be helpful. Many people experience temporary pain relief with moist heat treatments, massage, and topical creams. Physicians utilize medications and injections to decrease inflammation and joint stiffness.
Physical therapists perform joint mobilization techniques and prescribe gentle range of motion exercises to achieve the same goals. All of these treatments are very beneficial in the short term but by themselves will not result in any long-lasting changes.
How to Exercise In Spite of Pain to Decrease Pain
The longer you experience pain, the more sensitive you become to experiencing more and more pain. Contrary to popular belief, people with chronic pain from arthritis have low pain thresholds. They actually begin to experience pain when little threat or danger is present. Their body’s nervous system has been put on “high alert” to protect itself.
In this case, the body’s protective mechanisms are failing and becoming detrimental to its own health. This is not a permanent state. You can desensitize your pain systems with some practice, patience, and a greater understanding of how pain works.

You must accept the fact that all pain is not a sign of damage. Some pain is acceptable when you are exercising with arthritis. The body and mind will never become less sensitive if all your actions are based on avoiding pain.
Instead, focus on the activity you would like to do like walking or gardening. Perform the activity in small doses at first. Walk for a few minutes each day for the first week. Don’t overdo it. Then add a minute or 2 next week. Be patient. Gradually, your nervous system will become less sensitive to the activity, your muscles will become stronger and your pain will begin to decrease.
Take Action and Get Some Help
There is no cure for arthritis. However, by changing your beliefs and taking action you can overcome arthritis pain. This is not an easy endeavor. Many are unwilling to commit. These people jump from one treatment to the next seeking a quick fix. Joint replacements can work wonders for some. However, they are not without serious risk and the outcomes are not always as promised.
If you are looking for a different, more holistic approach, your physical therapist can help. Begin with the strategies discussed in this article. And if you need more help your physical therapist can be your guide. Give us a call and schedule an appointment with your physical therapist.


